
.jpg)
Asthma and chronic obstructive pulmonary disease (COPD) represent the leading chronic respiratory diseases of interest in the word, owing to their high prevalence and burden on the health system.
Care of these patients, undergoing frequent exacerbations, is a heavy burden on healthcare systems. In the last few years, large improvements in the management of asthma and COPD have been made, owing to new drugs and management strategies, and to the improvement of the nonpharmacologic treatment of COPD. There are still many unmet needs in the treatment of these diseases. In asthma, strategies to improve control should be implemented. There is a need to use more biomarkers to tailor treatment, in the assessment and choice of appropriate therapy, especially in severe patients. In COPD, there is growing evidence of individual differences in lung function decline rate and associated differences in appropriate management strategies. Early effective and prolonged bronchodilation can slow disease progression and reduce the frequency of exacerbations. New perspectives include the use of biologic drugs (anticytokine monoclonal antibodies) in selected categories of severe asthmatics, potential new inhibitors of chemokines and cytokines involved in the pathobiology of asthma and COPD, and a further improvement of current drugs and better implementation of management strategies, particularly in COPD patients.

“Bioethics” is a term with two parts, and each needs some explanation. Here, “ethics” refers to the identification, study, and resolution or mitigation of conflicts among competing values or goals. The ethical question is, “What should we do, all things considered?” The “bio” puts the ethical question into a particular context.
Bioethics is commonly understood to refer to the ethical implications and applications of the health-related life sciences. These implications can run the entire length of the bench-to-bedside “translational pipeline.” Dilemmas can arise for the basic scientist who wants to develop synthetic embryos to better study embryonic and fetal development, but is not sure just how real the embryos can be without running into moral limits on their later destruction. How much should the scientist worry about their potential uses?
Once treatments or drugs are in clinical trials involving human subjects, a new set of challenges arise, from ensuring informed consent, to protecting vulnerable research participants to guarantee their participation is voluntary and informed. Eventually, some of these new approaches exit the pipeline and are put into practice, where providers, patients, and families struggle with how to best align the risks and benefits of treatment with the patient’s best interest and goals. The added costs of new therapies inevitably strain available resources, forcing hard choices about how to fairly serve the needs of all, especially those already underserved by the health care system.
Questions in bioethics aren’t just for “experts.” Discussions of bioethical challenges take place in the media, in the academy, in classrooms, but also in labs, offices, and hospital wards. They involve not just doctors, but patients, not just scientists and politicians, but the general public.

A definition for patient safety has emerged from the health care quality movement that is equally abstract, with various approaches to the more concrete essential components. Patient safety was defined by the IOM as “the prevention of harm to patients.” Emphasis is placed on the system of care delivery that (1) prevents errors; (2) learns from the errors that do occur; and (3) is built on a culture of safety that involves health care professionals, organizations, and patients. The glossary at the AHRQ Patient Safety Network Web site expands upon the definition of prevention of harm: “freedom from accidental or preventable injuries produced by medical care.
Patient safety practices have been defined as “those that reduce the risk of adverse events related to exposure to medical care across a range of diagnoses or conditions.This definition is concrete but quite incomplete, because so many practices have not been well studied with respect to their effectiveness in preventing or ameliorating har
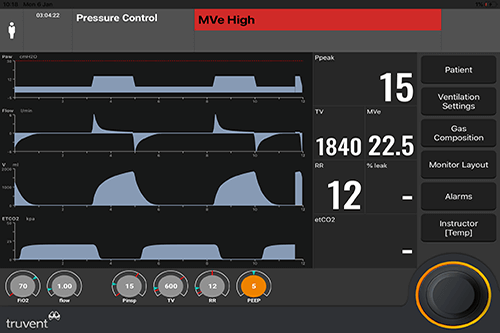
Intubation, with subsequent mechanical ventilation, is a common life-saving intervention in the emergency department (ED). Given the increasing length of stay of ventilated patients in EDs, it is necessary for emergency practitioners to have a good understanding of techniques to optimize mechanical ventilation and minimize complications.
Many different strategies of positive-pressure ventilation are available; these are based on various permutations of triggered volume-cycled and pressure-cycled ventilations and are delivered at a range of rates, volumes, and pressures. Poor ventilatory management can inflict serious pulmonary and extrapulmonary damage that may not be immediately apparent.

Noninvasive ventilation refers to the delivery of mechanical ventilation to the lungs using techniques that do not require an endotracheal airway. During the first half Read More
of the 20th century, negative pressure types of noninvasive ventilation were the main means of providing mechanical ventilatory assistance outside of the anesthesia suite. By the 1960s, however, invasive (i.e. via an endotracheal tube) positive pressure ventilation superceded negative pressure ventilation, primarily because of better airway protection. The past decade has seen a resurgence in the use of noninvasive ventilation, largely because of the development of nasal ventilation, which has the potential of providing ventilatory assistance with greater convenience, comfort, safety, and less cost than invasive ventilation. The following will explore these trends in the use of noninvasive ventilation and then provide a current perspective on applications in patients with acute and chronic respiratory failure. The discussion will consider the rationale for use, currently available techniques and equipment, evidence for efficacy, selection of appropriate patients, and general guidelines for application, monitoring, and avoidance of complications.

Critical care medicine encompasses the diagnosis and treatment of a wide variety of clinical problems representing the extreme of human disease. Critically ill patients require intensive care by a coordinated team. The critical care specialist (sometimes referred to as an “intensivist”) may be the primary provider of care or a consultant. The intensivist needs to be competent not only in a broad range of conditions common among critically ill patients but also with the technological procedures and devices used in intensive care settings. The care of critically ill patients also raises many complicated ethical and social issues, and the intensivist must be competent in areas such as end-of-life decisions, advance directives, estimating prognosis, and counseling of patients and their families.
Most physicians trained in critical care medicine work in hospital-based settings, usually in intensive care units. Within internal medicine, critical care medicine training is most commonly hidden content coupled with a pulmonary medicine fellowship since pulmonologists frequently oversee care of patients in intensive care units. However, other internal medicine physicians, such as cardiologists and general internists practicing hospital medicine, may seek training in critical care medicine to facilitate their work with severely ill patients.